The Process and Importance of Washer Disinfector Validation
Clean instruments, free of all infectious agents, are vital for dentists and surgeons. Using a washer disinfector before autoclaving is the accepted protocol. Any residual blood, pus or other bodily fluid on a dental drill bit or scalpel blade provides an ideal environment for the growth of microorganisms, and the fluids themselves could harbour virus particles or bacteria from a recent patient.
Immersion in a disinfectant doesn’t guarantee sterility as congealed proteins can form an impenetrable barrier, protecting bacteria from its effects. Also, some organisms can form spores, allowing them to remain dormant, insulated from disinfectants and all but extreme temperatures until external conditions are more favourable. For these reasons, it is necessary to thoroughly wash surgical and dental instruments before disinfecting them.
Washing by hand is time-consuming and less effective. Consequently, combined washing and disinfecting systems have become a cornerstone of the modern dental practice.
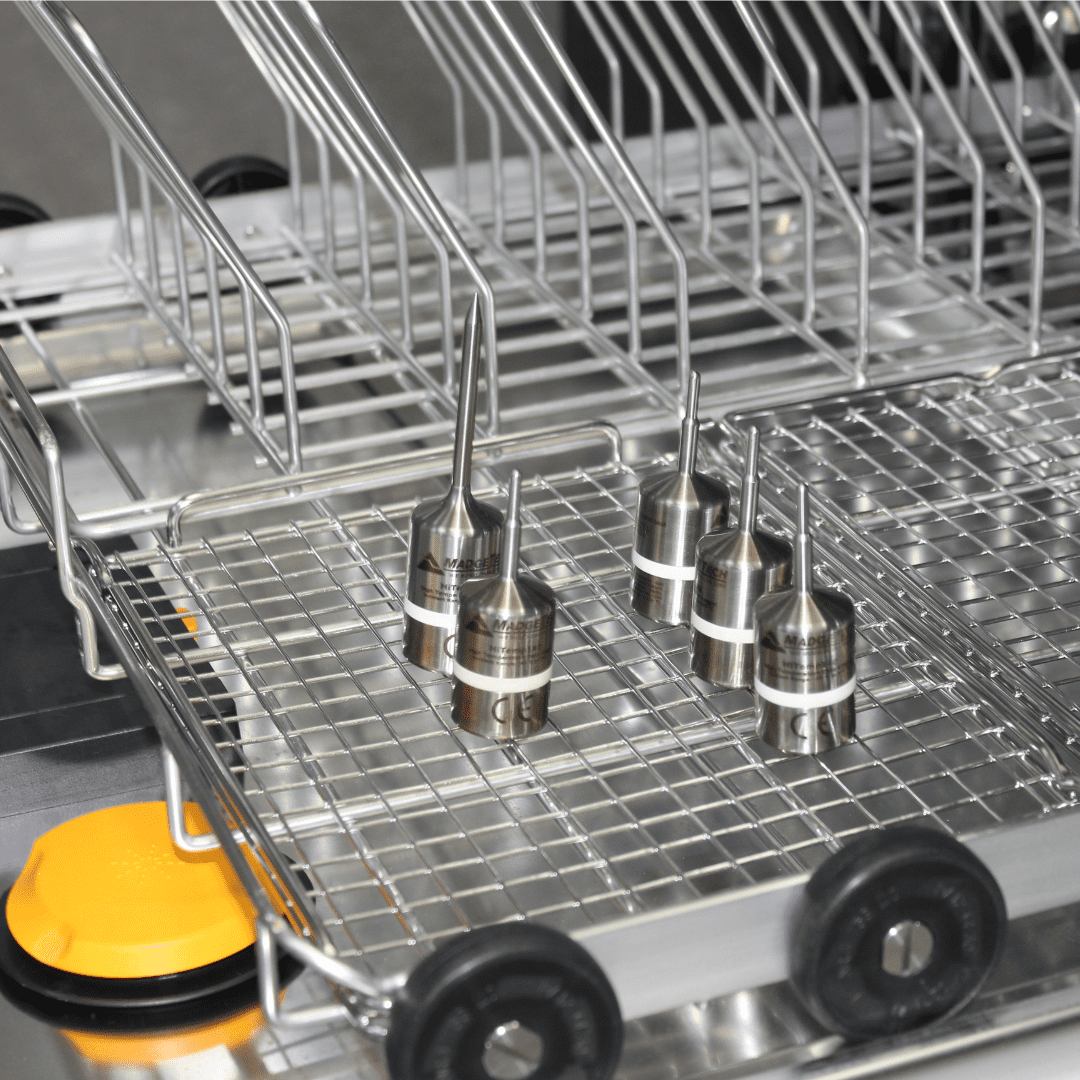
How the Dental Washer Disinfector Works
These systems employ a multistage process, combining mechanical action, thermal energy and detergents to clean and disinfect medical and dental instruments. The sequence of events is as follows:
- Pre-wash: The instruments are first rinsed to remove loose debris.
- Cleaning: A combination of high-pressure water jets and detergent is used to remove any residual organic and inorganic material.
- Rinsing: In this step, the instruments are rinsed to remove all traces of the detergent.
- Thermal disinfection: Water is heated to produce steam, increasing the temperature in the chamber to 80 degrees Celsius. Exposure for at least a minute is sufficient to denature most pathogens.
- Drying: In this final stage, the instruments are dried in hot air to prevent recontamination, leaving them ready for immediate use or, wherever possible, autoclaving for use later.
The cycle is controlled by a software programme that ensures consistent and repeatable performance, reducing the risk of human errors common with manually operated systems. However, even automated equipment is prone to occasional failures. Consequently, periodic medical washer disinfector validations are essential to ensure patient safety.
Dental Washer Disinfector Validation Tests
Validation is required as per the manufacturer’s recommendation and the validation cycle may vary. The process involves specialised testing of crucial stages in the washing and disinfecting cycle. Should a system fail, it must be removed from service immediately. Validation should be conducted by a qualified dental engineer and include the following key tests:
- Soil test: Treated instruments are inspected visually and analysed with colour-changing chemical indicators for any trace of residual soil following a completed cycle.
- Protein residue: Residual protein on an instrument can harbour bacteria. This test uses swabs and culture media or chemical indicators to determine whether post-wash protein levels are within acceptable limits.
- Thermal disinfection test: The engineer uses temperature sensors or biological indicators containing heat-resistant spores to ensure the system can reach and maintain the specified temperature for the required time.
- Spray-arm test: This procedure involves checking mechanical actions, like smooth spray rotation and water jet pressure.
- Automatic control test: This tests the mechanisms that regulate timing, temperature, detergent dosing, and initiate each function.
Booking a Medical Washer Disinfector Validation
Hague Dental Supplies has a team of qualified and experienced engineers skilled in installing, maintaining, repairing and validating dental equipment. Contact us to cover all your dental validation requirements and ensure your patients’ safety.